A 38-year-old Haitian woman presents to a Florida emergency department in April 2018 reporting pain on the right side of her abdomen, where she can feel a large lump. She tells clinicians she has had significant swelling in her abdomen, despite experiencing weight loss.
After palpation of her abdomen confirms the presence of a large mass, clinicians order a CT scan. This reveals a large complex cyst in the lateral right lobe of the liver measuring 21.9 × 14.4 × 17.3 cm.
They drain the cyst laparoscopically, removing 2,000 cc of brown-red fluid. Clinicians initially consider several possible differential diagnoses, including bacterial and parasitic infections. Biopsy serology findings are negative for Echinococcus and Entamoeba IgG, and cultures are unremarkable.
The patient’s medical history dates back to 2014, when she presented to the same hospital with a large ameloblastoma in the angle of the mandible measuring over 30 cm AP × 30 cm across and weighing over 1 kg. This had gradually spread to her jaw, neck, and floor of her mouth.
The mass was comprised of soft tissue and numerous ossifications. It had spread to involve her mandibular molars and premolars, and protruded from her mouth with floating teeth, severely affecting the patient’s ability to speak and to eat.
Although the tumor had not invaded her maxillary teeth and tongue muscles, its size interfered with full range of motion of the patient’s lingual muscles. It occupied the whole jaw from angle to angle, down to the lower tracheal region, and forced the lower lip downward to her chest.
The patient underwent surgery that year to remove the mass. Cytology test results revealed a lack of significant atypia, and stained positive for cytokeratin 5/6 and P63. Morphological analysis identified odontogenic epithelial islands without dentin or enamel formation, suggesting a diagnosis of primary malignant ameloblastoma.
Following the surgery, the patient developed a left-sided deep vein thrombosis and pulmonary embolism. Clinicians placed an inferior vena cava filter. However, the patient returned to Haiti without receiving the indicated anticoagulation therapy.
Two years later, in 2016, she developed another mass, which was surgically removed at the same medical center. Although malignancy recurred, affecting the floor of her mouth, deep strap muscles of her neck, and minor salivary glands, clinicians did not find any signs that it had infiltrated her jaw.
Clinicians observed the mass to be highly vascular and growing very rapidly. The recurrent tumor was about a third of the size of the original, and involved only soft tissues.
Clinicians note that the patient is not a smoker or drinker, has no allergies, and no family history of cancer.
When she presents to the emergency department in 2018, the liver cyst fluid is positive for cytokeratin 5/6, P63, and CD56, which indicates metastasis of malignant ameloblastoma (Figure).
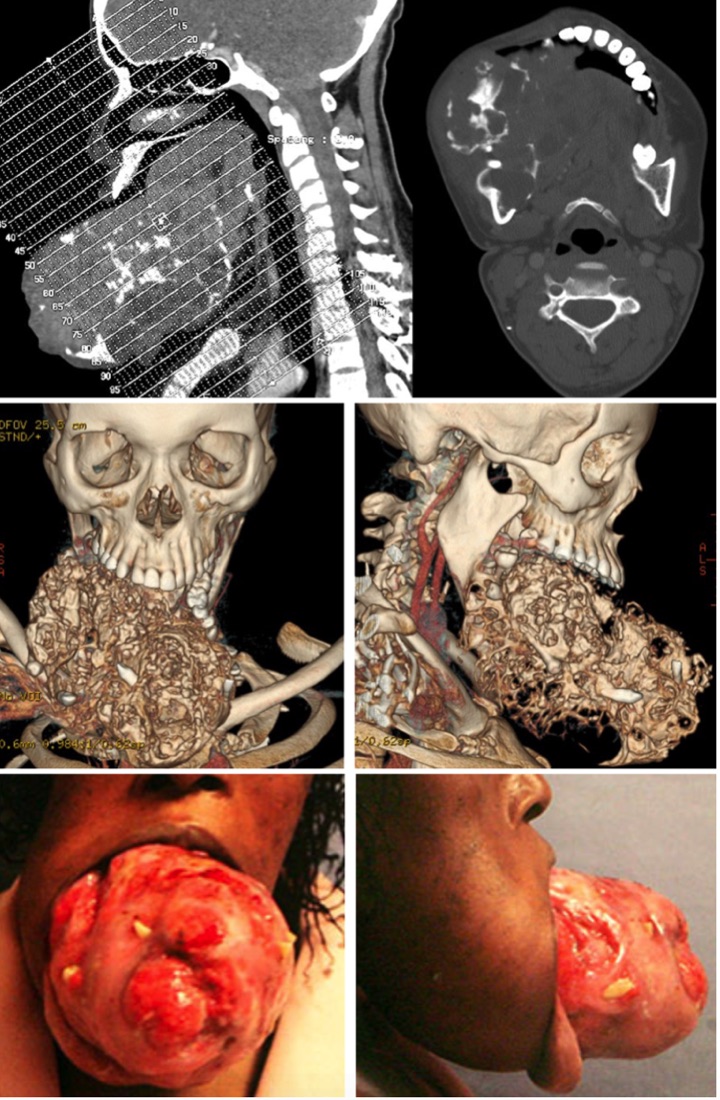
CT imaging of primary ameloblastoma with measurement and three-dimensional reconstruction.
As with analysis of the patient’s earlier masses, the cystic cells show odontogenic epithelial islands, but not dentin or enamel formation.
Following drainage, the patient’s corrected serum calcium increases to 13.3 and clinicians start her on calcitonin. Three days after the surgery, she develops dyspnea. A CT pulmonary angiogram shows no evidence of a pulmonary embolism; however, there is re-accumulation of intrahepatic fluid within the right lobe and right hemidiaphragm elevation with submaximal inspiration.
Before her respiratory symptoms are fully resolved, the patient returns to Haiti and she does not return for postoperative care or chemotherapy. She dies in 2020; in the absence of a post-mortem autopsy, her death is suspected to be related to complications of the metastatic ameloblastoma.
Discussion
Clinicians presenting this case of a 38-year-old woman with a highly aggressive recurrent malignant ameloblastoma involving the mandible and floor of the mouth — which ultimately metastasizes to her liver — note that only about 100 such cases have been reported since it was first described almost 100 years ago.
Ameloblastomas arise from the dental lamina epithelium, and generally occur as either a benign or malignant ameloblastoma. Malignant ameloblastomas are very rare, constituting less than 2% of all odontogenic tumors and roughly 4% of ameloblastomas, case authors note. They were categorized by the WHO in 2005 as ameloblastic carcinoma and malignant ameloblastoma. “Unlike malignant ameloblastoma, ameloblastic carcinoma presents with significant cytological atypia, increased mitoses with atypical forms, and a high N:C ratio,” case authors write.
While age at diagnosis of ameloblastoma ranges from 5 to 74 years, case authors note that the average age at diagnosis is 34, with incidence evenly divided between men and women.
This particular patient’s case “followed an atypical malignant ameloblastoma pattern,” authors note; just 2 years after the primary mandibular tumor was radically excised, a very aggressive, fast-growing, and highly vascular lesion developed on the floor of the patient’s mouth. Cytology results showing positive staining for cytokeratin 5/6, P63, and CD56 were in keeping with typical features of ameloblastoma, allowing clinicians to confirm the diagnosis of hepatic metastatic malignant ameloblastoma.
Primary ameloblastoma most often develops at the angle of the jaw, while the maxilla is less frequently involved, case authors note. Metastasis frequently occurs after several local recurrences, most frequently through a hematogenous route to the lungs (75-88%); the second most common site is the cervical lymph nodes, and other less common sites include vertebrae, pleura, skull, parotid gland, diaphragm, and liver.
Case authors report that cough, dyspnea, and hemoptysis may be presenting symptoms of lung involvement, which more rarely may present with paraneoplastic syndrome. Lung metastases are often slow to show clinical progression, and they tend to have long median survival times.
In contrast to this patient’s case, “ameloblastomas are often described as slow-growing with a high likelihood for local recurrence,” authors observe, although local recurrence follows treatment in about half to three-quarters of patients. Thus, postoperative follow-up is a necessity in ameloblastoma management.
“Although the recommended therapy for localized cases is surgical resection, the anatomical complexity of the mandibular region often causes difficulty for attaining recommended surgical excision margins,” authors write. Incomplete resection may be followed by adjuvant radiotherapy where appropriate.
Unfortunately, there are no established treatment regimens for metastatic ameloblastoma; outcomes associated with radiotherapy and chemotherapy have been unpredictable, authors note.
Therapies demonstrating some activity include cisplatin combined with cyclophosphamide, vinblastine, bleomycin, paclitaxel, and carboplatin, they add. The rarity of metastatic ameloblastoma makes trials of treatment approaches impractical. Nevertheless, patients may survive a median 17.6 years after diagnosis, with survival decreasing as age at diagnosis increases.
This patient’s return to Haiti after each surgery and after drainage of the liver cyst meant she had more difficulty accessing appropriate local medical care and follow-up, leading to the severe progression of the initial primary ameloblastoma and recurrence.
Conclusion
This case demonstrates the importance of obtaining a detailed medical history to determine the etiology of these rare diseases, case authors conclude, adding that after initial treatment, “establishing frequent follow-up to manage disease progression can limit the extreme development seen with this patient.”
Last Updated July 02, 2021
-
Kate Kneisel is a freelance medical journalist based Belleville, Ontario.
Disclosures
The authors had no conflicts to disclose.
