The share of candidates who pass the licensure exam to work as a registered nurse has significantly dropped in recent years, and the National Council of State Boards of Nursing (NCSBN) — the regulator tasked with overseeing the exams — has no plans to make it any easier.
Most leading nurse academics say that’s a good thing. “Both as a nurse, but also as a potential patient, I want nurses to be highly qualified,” said Linda Aiken, PhD, RN, founding director of the Center for Health Outcomes and Policy Research at the University of Pennsylvania School of Nursing in Philadelphia. “I don’t think anybody in the public is interested in lowering standards for nurses,” especially not after seeing the role that nurses played during the COVID-19 pandemic.
Falling Pass Rates
The percentage of U.S.-educated candidates taking the National Council Licensure Examination for registered nurses (NCLEX-RN) for the first time and passing fell from 88.2% in 2019 to 82.5% in 2021, while the pass rate for all candidates (including internationally educated and repeat candidates) fell from 72.8% to 68.9%.
Pass rates continued to decline in 2022, with an average pass rate of 80.9% for all first-time U.S.-educated candidates, and a rate of 66.6% for all candidates, based on a dataset that excludes the fourth quarter of the year.
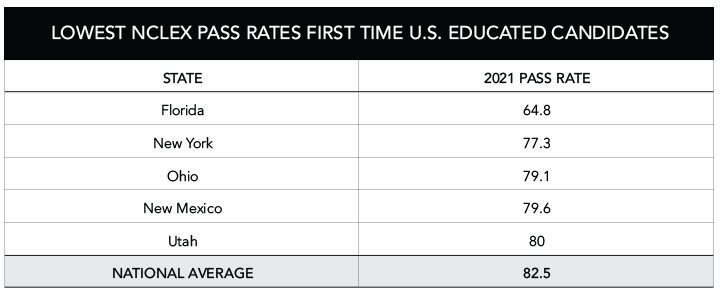
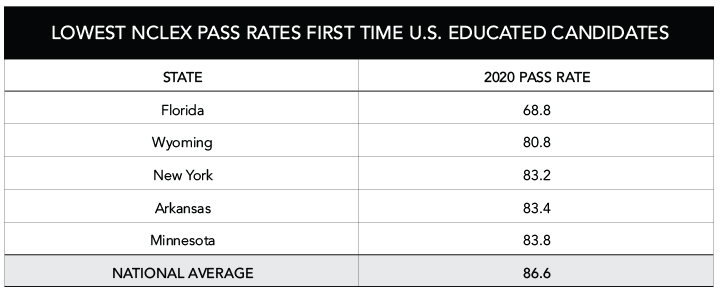
Of note, certain states’ pass rates are markedly lower than others. Florida ranked the lowest in the nation for first-time pass rates among U.S.-educated candidates in 2020 and 2021, with a rate nearly 18 percentage points below the national average.
Wyoming and New York had the second and third lowest pass rates in 2020, while New York and Ohio had the second and third lowest rates in 2021. However, the gap between the national average and each of these states has been at most 5 to 6 percentage points — far narrower than the margin between national pass rates and Florida’s rate.
The Pandemic’s Impact
Nearly every source that MedPage Today spoke to for this story, including the NCSBN, agreed that the pandemic has had an outsized impact on NCLEX pass rates over the past 3 years, in addition to other factors. “Clinical placements were limited and sometimes eliminated from the curriculum” because of COVID-19, said Dawn Kappel, director of marketing and communications for the NCSBN.
The decision to suspend clinical rotations for thousands of students at New York hospitals and other health facilities in March 2020 had a “devastating” impact on nursing education, an official from New York State’s Education Department told MedPage Today in an email. Many facilities didn’t have enough personal protective equipment to protect students, and others were restricting the number of people on campus to prevent transmission of the virus, the official said.
Given the full year and a half without clinical rotations, “it is not surprising that the pass rates on the nurse licensing examinations have declined,” the official added.
For nursing students, ending clinical rotations meant they weren’t able to go into hospitals and receive the hands-on experience that they usually would have. This led to many nurses receiving the bulk of their clinical training through simulation, explained Lori Hart, PhD, APRN, executive director of the Wyoming State Board of Nursing. While research supports substituting up to half of traditional clinical hours with high-quality clinical simulation, there’s “a downside” when 100% of a student’s clinical training is simulated, Hart noted.
The second change was the “quick pivot” to online education, said Maria Flores-Harris, DNP, MSN, BSN, RN, former executive director of nursing for Kaplan Test Prep in New York City, who has since started her own consulting business, Academic Partners Consulting. Online education has its place, she added, but neither students nor faculty were prepared for such a rapid transition. “And so during that time … students were not engaged. They were not doing the work.”
The NCSBN launched a study of dozens of nursing education sites across the country to better understand the pandemic’s effects on nursing education, as well as to track students’ performance and assess the effectiveness of new approaches to preparing students for the transition to the workforce, Kappel told MedPage Today. That report is slated for release in April.
Other Challenges: Less Oversight, Faculty Turnover, Leadership Changes
Wyoming had the second lowest pass rate in the country in 2020. But in 2021, Wyoming’s pass rate for first-time U.S.-educated candidates bounced back and outpaced the national average, though by only a hair (83.1% vs 82.5%). Apart from the pandemic itself, Hart attributed the state’s lower pass rates to challenges finding and retaining qualified faculty to serve in the least populated state in the country. The fact that faculty salaries are lower in rural areas also doesn’t help, she said.
To help address the situation, Wyoming is currently leveraging information about “warning signs” — including faculty turnover, leadership changes, and new program status — gleaned from a 2020 NCSBN study in the Journal of Nursing Regulation, to flag problems before they get worse.
According to the study authors, “frequent director turnover resulted in significant statistical differences in the NCLEX pass rates and differences in program approval status.”
Hart noted that, in Wyoming, programs that have not met the 80% first-time pass rate are given a “plan of correction.”
MedPage Today also contacted the boards of nursing for New York and Ohio — two of the states with the lowest NCLEX-RN pass rates for first-time U.S.-educated candidates in 2021. New York’s Department of Education said only that while the urgency around the pandemic has decreased, there are still challenges and it “continues to work to support [New York state] nursing schools and ensure that nursing students are prepared for safe entry-level practice.” A spokesperson for the Ohio Board of Nursing did not comment on the reasons for the decline in pass rates.
Do NCLEX Pass Rates Matter?
Every state has its own nursing board and each one sets its own requirements with regard to the NCLEX, explained Flores-Harris. Some states want every program to have a pass rate equal to or above the national pass rate, other states say a school must be within 5 percentage points, and still other states require 10 percentage points.
“But if you’re looking for a common denominator, it is that national NCLEX pass rate that everybody is looking at and using as the benchmark,” Flores-Harris said.
In a 2020 editorial published in Teaching and Learning in Nursing, Marsal Stoll, EdD, MSN, RN, CEO of the Accreditation Commission for Education in Nursing (ACEN), noted that “the vast majority of nurse educators support the use of first-time licensure pass rates as an important outcome measure reflective of program quality,” citing what were at that time “recent revisions to the ACEN standards and criteria.”
But NCLEX pass rates aren’t the full picture, Flores-Harris said. “If a school is bragging that they have 100% NCLEX pass rates, but only 30% of their students are getting through the program, is that really much to brag about?”
Other ways to assess a school’s performance include looking at graduation rates, attrition rates, and the employment rate of its students (although, given the current demand for nurses, Flores-Harris said she doubted any graduate would have difficulty finding a job).
Approval by the state’s board of nursing or accreditation by an accrediting organization also are regarded as measures of quality. “Accreditation really looks at the full program [including having qualified faculty, an appropriate curriculum and testing] and when you have a stamp … of accreditation, that does mean that you’ve met more rigorous standards than just an approved program through the Board of Nursing,” said Flores-Harris.
Retaining Passing Standards
The NCSBN routinely evaluates pass rates for the NCLEX every 3 years. The council conducts what is called a practice analysis — sending surveys to employers, educators, and thousands of nursing students — that includes questions about newly graduated nurses’ tasks, including how frequent these tasks are, how important they are, and whether they require clinical judgment, Flores-Harris explained. That information is used to determine whether the current test questions are still relevant or need to be more rigorous, she added.
If the NCSBN believes that the clinical judgment necessary for what nurses are doing has increased since the last time they raised the passing standard, then they will raise it again. If they feel the passing standard is “at a sufficient level that … if a candidate passes this exam, they are safe to practice as a nurse,” then they maintain the current standard, Flores-Harris said.
Last month, the NCSBN’s Board of Directors held a vote and “determined that the current passing standard is appropriate as a measure of safe and effective entry-level nurse practice,” said Jay Douglas, MSM, RN, the board’s president, who is also executive director of the Virginia Board of Nursing, in a press release. The council decided to uphold passing standards for both the NCLEX-RN and the NCLEX-PN, the exam for licensed practical nurses.
Separately, for the last few years, the NCSBN has been updating the original NCLEX and in its place plans to offer the Next Generation NCLEX (NGN) based on “a recognition that clinical judgment underpins almost everything nurses do,” Kappel said, adding that the NGN aims to “more effectively measure” clinical judgment of students taking the exam.
According to Flores-Harris, one of the biggest changes with the NGN is the inclusion of case studies, for which students are shown a patient’s electronic chart and asked questions about the patient. The NGN is expected to launch on April 1.
-
Shannon Firth has been reporting on health policy as MedPage Today’s Washington correspondent since 2014. She is also a member of the site’s Enterprise & Investigative Reporting team. Follow
Please enable JavaScript to view the
