Adjunctive left atrial appendage (LAA) ligation failed to increase the efficacy of catheter pulmonary vein isolation (PVI) in the aMAZE trial, though it appeared safe enough for further clinical investigation.
In a population of people with nonparoxysmal atrial fibrillation (Afib), LAA ligation plus PVI was associated with no better primary effectiveness by 12 months — or freedom from documented atrial arrhythmias lasting >30 seconds — than PVI alone (64.3% vs 59.9%, posterior superiority probability 0.835), reported researchers led by Dhanunjaya Lakkireddy, MD, of Kansas City Heart Rhythm Institute and University of Missouri-Columbia.
The trial showed a 3.4% rate of composite serious adverse events at 30 days, which was well within the prespecified safety goal of 10%. The safety events recorded were eight bleeds, three cardiac injuries, and one vascular injury in the roughly 600-person study.
“Stroke prevention was not a study end point, but future studies for this outcome are warranted because the device appears to be effective for left atrial appendage exclusion and the safety performance goal of the trial was met,” the authors wrote in JAMA.
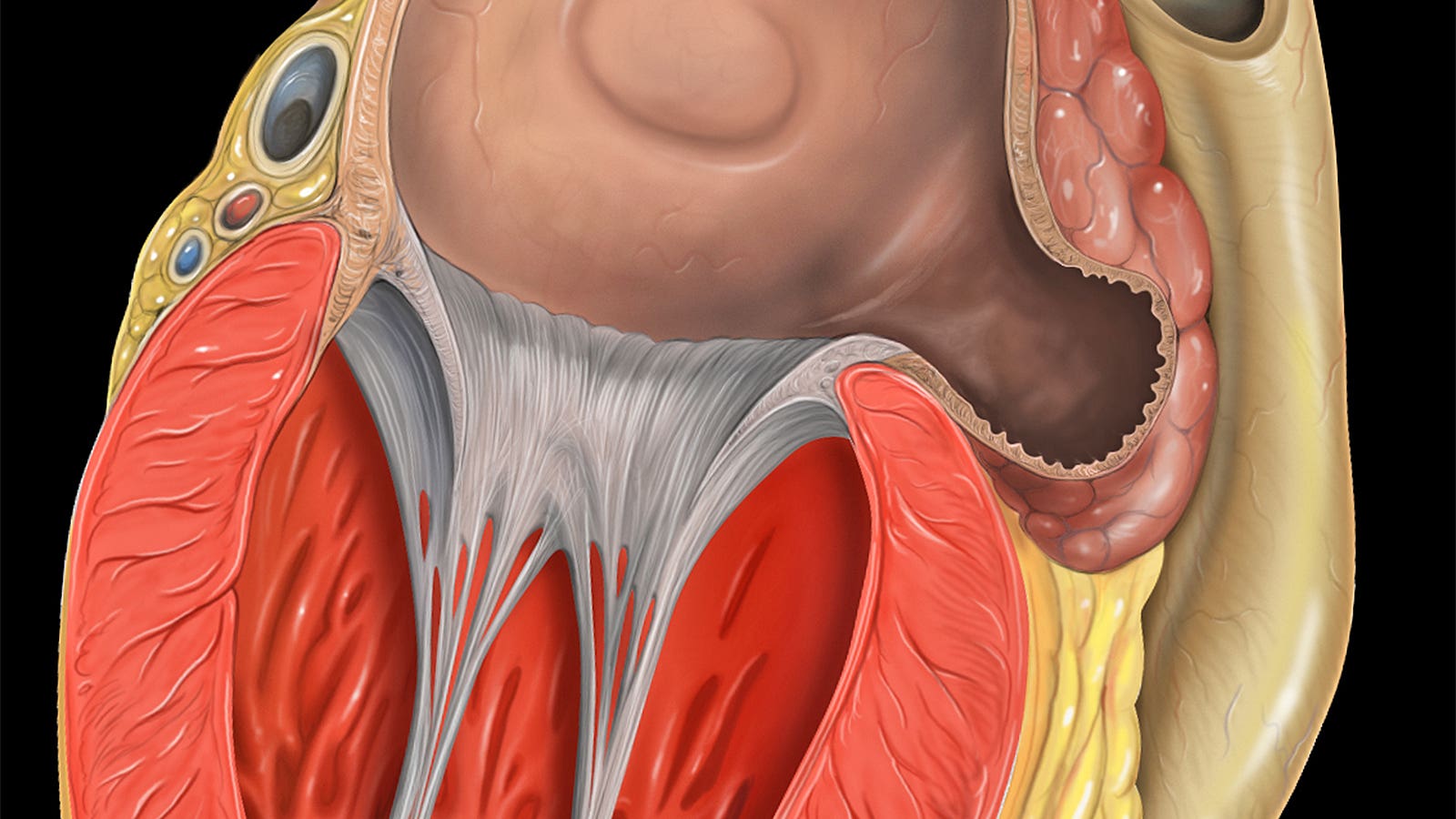
The manuscript is now finally published years after aMAZE’s main results had been presented at the 2021 meeting of the American Heart Association. The trial tested percutaneous LAA ligation using the Lariat single-use device that delivers a pretied polyester suture loop to the epicardial heart surface. Patients in the intervention group underwent a 30-day follow-up visit for clinical assessment and transesophageal echocardiography, and then pulmonary vein isolation within the next 30 days.
Lariat developers are also now trying to make the case for a staged “Convergent” Afib ablation procedure, in which the patient undergoes epicardial ablation with a concomitant Lariat LAA ligation, followed by endocardial radiofrequency catheter ablation. This is being tested in the small CLIP-AF trial currently underway.
Moreover, with additional patients enrolled through aMAZE’s continued access protocol, investigators recently reported some evidence that the subgroup of Afib patients with a larger volume of the left atrium (>130 cc), likely due to adverse atrial remodeling, was more likely to benefit from LAA ligation.
“I think this data is being presented to FDA, so we’ll see what comes out of that,” Lakkireddy told the Arrhythmia & Electrophysiology Review in February. “I really believe that there should be a specific indication in patients with large left atria with non-paroxysmal atrial fibrillation, they should be allowed to have a Lariat ligation.”
The aMAZE Study authors made it a point to distinguish the LAA ligater from other LAA occluders that are not designed to result in LAA necrosis.
“This trial was based on the premise that left atrial appendage ligation creates left atrial appendage ischemic necrosis, atrophy, and resorption leading to left atrial appendage electrical isolation and a reduction of left atrial appendage tissue,” Lakkireddy’s group wrote.
aMAZE was an open-label trial conducted at 53 U.S. sites. Participating patients had nonparoxysmal Afib for less than 3 years and needed to have a record of unsuccessful treatment with at least one class I/III antiarrhythmic drug. They were randomized 2:1 to LAA ligation plus PVI (n=404) or PVI alone (n=206) from 2015 to 2019. After dropouts, investigators had 378 and 198 people in those groups, respectively, for the primary analyses.
Median age was 68 years in LAA ligation and control groups. Patients were over 70% men and over 93% white. The group reported an average 4.7 months of Afib, with 13% having a diagnosis of long-standing persistent Afib. Left atrial volume was a median 131.8 mL in the LAA ligation group and 137.9 mL in the control group.
Rhythm was assessed by a combination of Holter monitoring at 6 and 12 months after PVI, symptomatic event monitoring, or any ECG tracing obtained through 12 months after PVI.
The durability of LAA closure was assessed at 12 months post-PVI, at which point 84% of people had complete LAA closure, and 99% no more than a 5-mm residual leak, according to Lakkireddy and colleagues.
Study limitations included a lack of assessment of left atrial appendage electrical isolation and its relationship to closure.
“Investigators bias to target non-pulmonary vein substrate in late persistent and long-standing persistent atrial fibrillation may have reduced enrollment of those patients for whom left atrial appendage ligation benefit may be expected to be more prominent, thus diluting overall treatment effect,” Lakkireddy’s group also cautioned.
-
Nicole Lou is a reporter for MedPage Today, where she covers cardiology news and other developments in medicine. Follow
Disclosures
aMAZE was funded by AtriCure.
Lakkireddy disclosed consulting for Abbott, Acutus, AltaThera, AtriCure, Biotronik, Boston Scientific, Biosense Webster, Lifetech, Medtronic, Philips, and Sanofi. Co-authors reported multiple relationships with industry.
Primary Source
JAMA
Source Reference: Lakkireddy DR, et al “Pulmonary vein isolation with or without left atrial appendage ligation in atrial fibrillation: the aMAZE randomized clinical trial” JAMA 2024; DOI: 10.1001/jama.2024.3026.
Please enable JavaScript to view the